
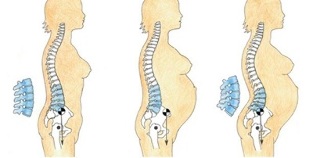
Older people, professional athletes, as well as those whose job involves sitting or standing without standing for long periods of time, are often exposed to various diseases of the musculoskeletal system. Irrational daily menu, physical inactivity leads to consumption, destruction of bones and cartilage. As a result, osteochondrosis of the lumbar spine develops, the symptoms and treatment of which depend on the personal characteristics of the organism, as well as the severity of the lesion.
According to the International Classification of Diseases of the 10th revision, this disease was assigned the code M42. Sometimes patients are given difficult diagnoses, coding simplifies the work of doctors. This short alphanumeric designation can be recorded in the medical history, outpatient card. So what is osteochondrosis of the lumbar spine? What are the reasons for its occurrence? What are the manifestations of the disease? This publication tells the story of everything.
Causes of lumbar osteochondrosis
Osteochondrosis of the lumbar spine often causes trauma and a sluggish lifestyle. Among other things, one of the main roles is played by the charged inheritance, as well as the hormonal, chemical, psychogenic background of the body.
If parents have suffered from lumbar osteochondrosis, the symptoms and treatment are likely to show up and pass on to their children. By inheriting predisposing factors, offspring are also at risk of developing this disease.
Provoking factors include the following reasons for the occurrence:
- Other diseases, such as digestive tract, liver, pelvis, nervous system;
- Step towards slowing metabolism;
- Shift of acid-base balance towards oxidation (acidosis);
- Reduce engine power;
- Stress, nervous situation;
- Long difficult postures, incorrect behavior.
Often, sacral osteochondrosis occurs as a result of hypothermia, hormonal disruption, or as a result of congenital pathological spinal defects.
Symptoms of lumbar osteochondrosis
Signs of lumbar osteochondrosis are associated with the fact that the spinal nerve fibers pass into the posterior area within the spinal canal. Depending on the localization, the severity of damage to some roots, the manifestations of the disease vary.With osteochondrosis of the lumbar spine, the following symptoms stand out:
- Pain Syndrome- most patients complain of low back pain in osteochondrosis. The pain is local directly to the area of the lesion, or radiates to the gluteal region, the sacrum of the foot on the side of the lesion;
- Tension sign- grief increases with a certain position, but when the body position changes, the pain suddenly disappears. The most commonly used test is named after the detector - Lasegue syndrome - the pain increases when the right limb is lifted up, and disappears when the leg is bent at the knee;
- Decreased or increased sensitivity- this symptom is directly related to the defeat of the radicular nerves, the sensitivity is not disturbed instead of localizing the pathology, but at some distance. The patient has hypesthesia, hyperesthesia or paresthesia, which is characterized by unusual projection sensations, such as goose bumps, tingling sensation, etc.
Often, with lumbar osteochondrosis, motor activity decreases, this is accompanied by muscle atrophy to varying degrees. In some circumstances, there is a limitation of functions, in other situations paralysis and paresis occur.
Also, lumbar chondrosis is associated with damage to the spinal vessels, with their irritation and spasm, vegetative changes appear. Blood circulation in the legs slows down, the lower extremities freeze constantly, there is a fading of the skin. Other organs in the lumbar region are often affected. So, with bladder damage, urinary incontinence develops or, conversely, is delayed.
Stages of the disease
- First degree lumbar osteochondrosis is the initial type of pathology. It is characterized by a low density of intervertebral discs. Pain syndrome manifests itself with a sharp twist of the body, after physical exertion or prolonged sitting.
This type of disease is common in drivers, office workers, athletes and people working in harsh climates. The pain is not characterized by acute attacks, but develops as a weakened or aching deafness.
At this stage, people do not rush to go to the doctors, but use traditional methods of treatment, such as oils, compresses. The situation leads to the fact that osteochondrosis of the lumbar or sacral spine passes into the second stage;
- Second degree lumbar osteochondrosis - degenerative and dystrophic disorders of the vertebral joints occur. The fibrous spinal ring is compressed, as the pulposus nucleus grows and elongation (elongation) of the intervertebral disc occurs.
Neuropathologists define the second stage of osteochondrosis as lumbago. In other words, a lumbago occurs in the lower back when a heavy object is lifted suddenly or with other loads. This period lasts for many years, alternating remission phases with acute attacks of exacerbations;
- Grade 3 osteochondrosis - pulp elongation gradually increases, an intervertebral hernia is formed. The patient develops the entire palette of neurological status: persistent pain, radiation to the buttocks, abdomen, tail bone, legs, urethra, limited mobility.
Legend is used to localize the hernia. Diagnosis of L5 S1 osteochondrosis means that swelling of the nucleus pulposus has occurred between the 5th lumbar vertebra and the 1st cruciate;
- When therapeutic measures are not taken in time, all stages of development proceed normally to the next stage. Stage 4 of lumbar osteochondrosis is characterized by the development of complications.
As a rule, drug treatment for highly developed pathology is characterized by low efficiency. The neuropathologist is obliged to offer a radical method of impact, namely hernia surgery.
Methods for the diagnosis of osteochondrosis
To identify EPP osteochondrosis, the neuropathologist first takes a medical history, because patient complaints are one of the crucial values for an accurate diagnosis. During the conversation, the patient is asked questions about his health and condition - what and where it hurts, what is the duration of the pain, what intensifies the feeling when stiffness appears, if the treatment has been performed, what it has been and the like.

Instrumental diagnostic methods are necessarily used:
- Overall Rg-graphic image of the lumbar spine- the spine is taken as a whole or its individual segments are photographed. More often than others, a targeted Rg-gram is made on the basis of complaints, in which the doctor notices disc atrophy, a decrease in the intervertebral space, the appearance of osteophytes, the mitigation of lumbar curvature;
- Myelography- contrast fluid is injected into the canal, where the spinal cord passes, using a spinal tap. The technique is used to determine the internal structure of the channel. Ordinary people consider the procedure as difficult and dangerous for diagnosis, but in addition to the allergy to contrast, the puncture in the spinal canal practically does not threaten the patient. Doing is done in the place where the spinal cord is missing;
- Computed tomography- determines the compression of nerve roots, determines the length of the pulp, it is easy to see the vertebral bodies, ligaments, vessels, soft tissues at close range on the monitor;
More precisely, sacral osteochondrosis is determined using electromagnetic waves, for which the patient is assigned an examination on a magnetic resonance scanner.
Each tissue has its own input signal, the computer processes the data and displays the image on the screen. The doctor examines the vessels, discs, bone processes, nerve fibers in a 1 mm incision. In this case, the patient does not receive harmful ionizing effects.
Treatment of osteochondrosis of the lumbar spine
Many patients are interested in the question: what to do with osteochondrosis of the lumbar region? Osteochondrosis of the lumbar spine does not always have indications for surgery. The main thing is that after a thorough examination of the patient, the usual therapeutic measures are sufficient.
Conservative therapy is reduced:
- For the treatment of medicines;
- Physiotherapy procedures;
- Gymnastic exercises from exercise therapy.
Also for the treatment of osteochondrosis of the lumbar spine, methods of manual therapy and methods from traditional medicine are used.
For the treatment regimen for osteochondrosis of the lumbar spine, the surgical method is offered to patients only in extremely severe cases, if conservative methods have not given the desired results.
Medications
Treatment of osteochondrosis of the lumbar spine is performed by a neuropathologist or the closest specialist, a vertebrologist. Before treating lumbar chondrosis of spinous processes, the doctor determines the stage and severity of pathological disorders.
Muscle relaxants are used to relieve pain, reduce spasm, inflammation. These medications quickly return movement to the patient, relieving spasms, so the pain goes away.
In addition to the group of drugs for muscle relaxation, steroid hormones are sometimes used to relieve swelling and inflammation.
Healing gymnastics
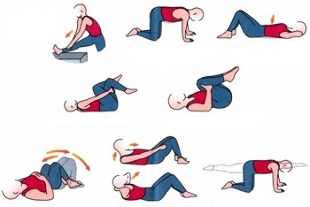
Treatment of lumbar osteochondrosis should be performed in conjunction with exercise therapy methods. Exercise and gymnastics should be given the same attention as the use of medication.
The therapeutic effect of osteochondrosis is those exercises that relieve pain, strengthen the muscular framework, reduce the pressure between the discs - this slows down the further progression of the disease.
Physiotherapy
In lumbosacral osteochondrosis, treatment involves the use of the following procedures:
- Electrophoresis with drugs;
- Laser and magnetic therapy;
- Magnetic current treatment;
- Darsonval;
- UV radiation;
- Diadine treatment;
- Shock wave method.
Manipulations involve the use of tools using natural physical force: currents, light radiation, vibrations, etc. The treatment regimen, the duration of the course for physiotherapy is determined by the attending physician.
Manual therapy
When a sick person asks a neurologist how to cure osteochondrosis of the lumbar spine using a manual technique, he is usually advised by a qualified specialist who, with his hands, not only affects the muscle tissue, butalso put the beads in place.
In case of lumbar chondrosis, this method normalizes blood and lymph circulation, eliminates muscle tone and deformation and restores motor function. Chiropractor hands reduce the purity of spasms, reduce back pain.
How is osteochondrosis of the lumbar region treated using manual techniques and is it possible to fully recover this way? Manual therapy is prescribed only when the degenerative processes have not disturbed the spinal tissues, i. e. no bone growths have been formed. The need for procedures is determined by the doctor after diagnosing Rg, CT or MRI.
Surgery
Treatment of lumbar chondrosis from surgery is performed according to certain indications, when the pathology is characterized by the following changes in the spine:
- The spinal canal narrows, the intervertebral discs are compressed and destroyed;
- Cauda equina syndrome develops - a massive bundle of nerves of the spinal cone, which irritates the pelvic region, the legs, is damaged;
- Loss of sensitivity progresses, there is a disorder of the ability of the internal organs to work;
- There is a risk of foot paralysis.
The operation is performed in accordance with emergency or scheduled indications. The goal of surgical treatment is to relieve pressure and improve the condition of the spine.
Traditional medicine
Treatment of lumbar spine osteochondrosis with popular methods is best done in consultation with your doctor.
People's Pharmacy offers many remedies to cure diseases:

- Medicinal plants, essential oils, flower extracts, plant roots;
- Animal products, such as snake or bee venom, badger, dog, sheep fat, boiled eggs and others;
- Iodine, turpentine and alcohol are used for heating, irritating effects.
Similar to medicine, chondrosis of the lower back is treated by folk methods only in the initial stage of the disease, while the symptoms are eliminated only, but the pathological changes do not disappear. Among other things, such a treatment often has side effects, because of this, a specialist consultation is required before using any prescription from traditional medicine.
The dosage of any medicine or medicine should be prescribed by your doctor.
Complications
Lumbar chondrosis in the last stage can lead to unpleasant consequences, including disability.
Against the background of dystrophy and degenerative disorders, a narrowing of the spinal canal is formed, stenosis develops. As a result of such changes, a chronic type of compression is formed, which interferes with normal blood flow, root ischemia or cauda equina syndrome develops.
Moreover, diseases such as spondylosis and spondyloarthritis sometimes develop - the intervertebral discs age, lose strength, and traction pain occurs due to the broken structure of the vertebral joints. Complications most often involve the crest of the lower spine, where bone growths similar to the spine are formed.In the third stage, as a complication of osteochondrosis, intervertebral hernias develop, diseases of the genitourinary system and other internal organs appear.
Preventive measures
Prevention of osteochondrosis of the lumbosacral spine is of no small importance. The lower back has the heaviest load, so you need to take special care of your back. It is worth remembering that regular gymnastic exercises are the key to a healthy back.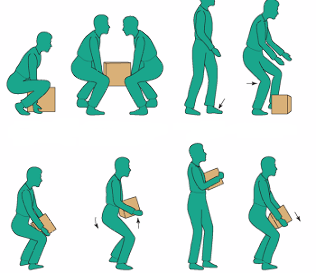
Weights should be lifted with the utmost care, avoiding sudden jumps. Men and women can carry burdens that are within reason.
Sitting in the office, you need to keep track of your posture, get the right posture and sit in a chair with your back straight. It is good to get up every hour and walk around the room, squat, turn the trunk: this eases the tension of the entire musculoskeletal framework.
Trigger point massage is excellent. They are active or are in a latent form. Trigger points appear as a result of overload, strong stretching, repetitive work, bending, hypothermia and other factors.
Knowing the reasons for the development of spasmodic areas, it is necessary to take measures to exclude their formation. Recently, a trigger point massager has gained popularity, it is better to prevent the appearance of painful foci with a special device than to treat them for a long time and expensive.























